Abstract
Purpose
Staphylococcus aureus is one of the most important hospital pathogens (involving wound infections) that can become resistant against antibiotics. This study aims to investigate the effects of Ferula gummosa (FG) essential oil on this bacterium during wound healing.
Methods
Ninety adult Wistar male rats were classified into five groups. After making wound in all rats, wound was infected by Staphylococcus aureus. Then, the control groups were treated with base ointment; and the third, fourth, and fifth groups were treated by base ointment containing 2%, 4%, and 8% of FG essential oil, respectively. On the 3rd, 7th, and 14th days, antimicrobial effects of FG essential oil against Staphylococcus aureus, as well as antioxidant biochemical factors, were tested on wound biopsies.
Results
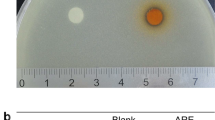
Antimicrobial test showed that FG essential oil caused decrement in Staphylococcus aureus infection. The levels of GSX, TAC, and SOD were significantly increased in FG essential oil–treated groups compared to the control group. Nevertheless, level of MDA was significantly less than that in treated groups in comparison to the control group.
Conclusion
Ferula gummosa has an antimicrobial effect on Staphylococcus aureus, and its local application can enhance the antioxidant activity in wound.
Lay summary
Ferula gummosa essential oil has antibacterial effects on skin infectious bacteria such as Staphylococcus aureus in vitro. Ferula gummosa has an antimicrobial effect on Staphylococcus aureus, and its local application can enhance the antioxidant activity in wound. It has locally been applied in the form of ointment and therapeutic doses. Staphylococcus aureus is one of the most important hospital pathogens (involving wound infections) that can become resistant against antibiotics. Increasing the levels of superoxide dismutase, glutathione peroxidase, and total antioxidant capacity as well as reducing of malondialdehyde and lipid peroxidation can inhibit cutaneous wound infected with Staphylococcus aureus, shorten the inflammatory phase, increase the proliferative phase, and increase the rate and quality of healing of infected wound in rats. Therefore, FG has been proposed to apply as antimicrobial agents with higher effect and lower toxicity in the cases of antibiotic resistance. However, more studies are needed to use it clinically.






Similar content being viewed by others
Data availability
Not applicable.
References
Treakle AM, Thom KA, Furuno JP, Strauss SM, Harris AD, Perencevich EN. Bacterial contamination of health care workers’ white coats. Am J Infect Control. 2009;37(2):101–5.
Chambers HF, DeLeo FR. Waves of resistance: Staphylococcus aureus in the antibiotic era. Nat Rev Microbiol. 2009;7(9):629–41.
Chambers HF. The changing epidemiology of Staphylococcus aureus? Emerg Infect Dis. 2001;7(2):178.
Ventola CL. The antibiotic resistance crisis: part 1: causes and threats. Pharmacy and therapeutics. 2015;40(4):277.
Orth D, Grif K, Erdenechimeg L, Battogtokh C, Hosbayar T, Strommenger B, et al. Characterization of methicillin-resistant Staphylococcus aureus from Ulaanbaatar, Mongolia. Eur J Clin Microbiol Infect Dis. 2006;25(2):104–7.
Cushnie TT, Lamb AJ. Antimicrobial activity of flavonoids. Int J Antimicrob Agents. 2005;26(5):343–56.
Simonetti G, Pucci N, Brasili E, Valletta A, Sammarco I, Carnevale E, et al. In vitro antimicrobial activity of plant extracts against Pseudomonas syringae pv. actinidiae causal agent of bacterial canker in kiwifruit. Plant Biosyst-An Int J Deal Asp Plant Biol. 2020;154(1):100–6.
Bahramsoltani R, Farzaei MH, Rahimi R. Medicinal plants and their natural components as future drugs for the treatment of burn wounds: an integrative review. Arch Dermatol Res. 2014;306(7):601.
Tindle HA, Davis RB, Phillips RS, Eisenberg DM. Trends in use of complementary and alternative medicine by US adults: 1997–2002. Altern Ther Health Med. 2005;11(1):42.
Neu HC. The crisis in antibiotic resistance. Science. 1992;257(5073):1064–73.
Kurahashi T, Fujii J. Roles of antioxidative enzymes in wound healing. J Dev Biol. 2015;3(2):57–70.
Mandegary A, Sayyah M, Heidari MR. Antinociceptive and anti-inflammatory activity of the seed and root extracts of Ferula gummosa Boiss in mice and rats. DARU J Pharm Sci. 2004;12(2):58–62.
Iranshahi M, Barthomeuf C, Bayet-Robert M, Chollet P, Davoodi D, Piacente S, et al. Drimane- sesquiterpene coumarins from Ferula gummosa fruits enhance doxorubicin uptake in doxorubicin-resistant human breast cancer cell line. J Tradit Complement Med. 2014;4(2):118–25.
Jalili-Nik M, Soukhtanloo M, Javanshir S, Yazdi AJ, Esmaeilizadeh M, Jafarian AH, et al. Effects of ethanolic extract of Ferula gummosa oleo-resin in a rat model of streptozotocin-induced diabetes. Res Pharm Sci. 2019;14(2):138.
Mazandarani M, Zeinali Z, Ghafourian M. Autecology essential oil composition, antibacterial, anti candidacies and ethnopharmacological survey of Ferula gummosa L. as anti infection to treat of vaginal infections in traditional medicine of Razavi Khorasan province (North East of Iran). Crescent Journal of Medical and Biological Sciences. 2015;2(2):42–47.
Burkatovskaya M, Castano AP, Demidova‐Rice TN, Tegos GP, Hamblin MR. EEffect of chitosan acetate bandage on wound healing in infected and noninfected wounds in mice. Wound Repair Regen. 2008;16(3): 425–431.
Kumar B, Vijayakumar M, Govindarajan R, Pushpangadan P. Ethnopharmacological approaches to wound healing—exploring medicinal plants of India. J Ethnopharmacol. 2007;114(2):103–13.
Benzie IF, Strain J. [2] Ferric reducing/antioxidant power assay: direct measure of total antioxidant activity of biological fluids and modified version for simultaneous measurement of total antioxidant power and ascorbic acid concentration. Methods Enzymol. 1999;299:15–27.
Lowry OH, Rosebrough NJ, Farr AL, Randall RJ. Protein measurement with the Folin phenol reagent. J Biol Chem. 1951;193:265–75.
Niehaus W Jr, Samuelsson B. Formation of malonaldehyde from phospholipid arachidonate during microsomal lipid peroxidation. Eur J Biochem. 1968;6(1):126–30.
Paglia DE, Valentine WN. Studies on the quantitative and qualitative characterization of erythrocyte glutathione peroxidase. J Lab Clin Med. 1967;70(1):158–69.
Nguyen NH, Tran G-B, Nguyen CT. Anti-oxidative effects of superoxide dismutase 3 on inflammatory diseases. J Mol Med. 2020;98;59–69.
Farahnak A, Golestani A, Eshraghian M. Activity of superoxide dismutase (SOD) enzyme in the excretory- secretory products of Fasciola hepatica and F. gigantica parasites. Iran J Parasitol. 2013;8(1):167.
Farahpour MR, Dilmaghanian A, Faridy M, Karashi E. Topical Moltkia coerulea hydroethanolic extract accelerates the repair of excision wound in a rat model. Chin J Traumatol. 2016;19(2):97–103.
Zhang Y, Yew W. Mechanisms of drug resistance in Mycobacterium tuberculosis [State of the art series. Drug-resistant tuberculosis. Edited by CY. Chiang. Number 1 in the series]. Int J Tuberc Lung Dis. 2009;13(11):1320–30.
Eftekhar F, Yousefzadi M, Borhani K. Antibacterial activity of the essential oil from Ferula gummosa seed. Fitoterapia. 2004;75(7–8):758–9.
Maggi F, Cecchini C, Cresci A, Coman MM, Tirillini B, Sagratini G, et al. Chemical composition and antimicrobial activity of the essential oil from Ferula glauca L.(F. communis L. subsp. glauca) growing in Marche (central Italy). Fitoterapia. 2009;80(1):68–72.
Ghasemi Y, Faridi P, Mehregan I, Mohagheghzadeh A. Ferula gummosa fruits: an aromatic antimicrobial agent. Chem Nat Compd. 2005;41(3):311–4.
Abedi D, Jalali M, Sadeghi N. Composition and antimicrobial activity of oleogumresin of Ferula gumosa Bioss. essential oil using Alamar Blue™. Res Pharm Sci. 2009;3(1):41–5.
Campos M, Calixto J. Neurokinin mediation of edema and inflammation. Neuropeptides. 2000;34(5):314–22.
Dabirmoghaddam P, Baradaranfar M, Gouinee F, Ayatallahi V. The effect of intravenous dexamethasone in reducing periorbital edema, ecchymosis and intraoperative bleeding in rhinoplasty patients. Tehran Univ Med J TUMS Publ. 2007;65(8):29–34.
Reilly PM, Schiller HJ, Bulkley GB. Pharmacologic approach to tissue injury mediated by free radicals and other reactive oxygen metabolites. Am J Surg. 1991;161(4):488–503.
Afshar FF, Saffarian P, Hosseini HM, Sattarian F, Amin M, Fooladi AAI. Antimicrobial effects of Ferula gummosa Boiss gum against extended-spectrum β-lactamase producing Acinetobacter clinical isolates. Iran J Microbiol. 2016;8(4):263.
Ates-Alagoz Z, Altanlar N, Buyukbingol E. Synthesis and antimicrobial activity of new tetrahydro- naphthalene-thiazolidinedione and thiohydantoine derivatives. J Heterocycl Chem. 2009;46(6):1375–9.
Rubio CP, Hernández-Ruiz J, Martinez-Subiela S, Tvarijonaviciute A, Ceron JJ. Spectrophotometric assays for total antioxidant capacity (TAC) in dog serum: an update. BMC Vet Res. 2016;12(1):1–7.
Bhoopathy J. Plant extract–derived nanomaterials for wound healing: a mini review. Regenerative Engineering and Translational Medicine. https://doi.org/10.1007/s40883-022-00265-y. Accessed 29 June 2022.
Islam M, Karmakar PC, Tusher Al A, Arifuzzaman M, Karim N, Akhtar N, et al. Human amniotic membrane and titanium dioxide nanoparticle derived gel for burn wound healing in a rat model. Regen Eng Transl Med. 2022. https://doi.org/10.1007/s40883-022-00280-z.
Verma YK, Verma R, Singh AK, Gangenahalli G. LiCl Containing Thermosensitive formulation improves hemostasis, wound healing, and hair regrowth. Regen Eng Transl Med. 2021;7(3):362–78. https://doi.org/10.1007/s40883-020-00148-0.
Banimohammad M, Ravaei H, Khalafi P, Javdan G, Ayatollahi SA, Davoodi SH. Change in total anti-oxidant capacity (TAC) of tissue, a new method for improving dermal wound healing. Sci J Kurdistan Univ Med Sci. 2019;24(3):96–109.
Nabavi SF, Ebrahimzadeh MA, Nabavi SM, Eslami B. Antioxidant activity of flower, stem and leaf extracts of Ferula gummosa Boiss. Grasas Aceites. 2010;61(3):244–50.
Farahpour MR, Mirzakhani N, Doostmohammadi J, Ebrahimzadeh M. Hydroethanolic Pistacia atlantica hulls extract improved wound healing process; evidence for mast cells infiltration, angiogenesis and RNA stability. Int J Surg. 2015;17:88–98.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study conception and design. Material preparation, data collection, and analysis were performed by Sahar Kalami, Najmeh Jooyan, Sahar Ghodsian, Omid Ghanbarpour, Amin Daemi, Masood Fardin, Mohammad R. Farahpour, Seyyedeh Touran Hosseini, and Yavar Yousefi. The first draft of the manuscript was written by Sahar Kalami, Najmeh Jooyan, Sahar Ghodsian, Omid Ghanbarpour, Amin Daemi, Masood Fardin, Mohammad R. Farahpour, Seyyedeh Touran Hosseini, and Yavar Yousefi, and all the authors commented on previous versions of the manuscript. All the authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal work protocols were approved by the Ethical Committee of Ardabil Branch of Islamic Azad University and with the approval of ethics code Irau.Ardabil.rec 1399.142.
Human and Animal Rights
All animal procedures were as per the guidelines of Islamic Azad University.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kalami, S., Jooyan, N., Ghodsian, S. et al. Ferula Gummosa a Good Candidate to Promote Cutaneous Wound Healing Infected with Staphylococcus Aureus. Regen. Eng. Transl. Med. 9, 547–557 (2023). https://doi.org/10.1007/s40883-023-00301-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40883-023-00301-5